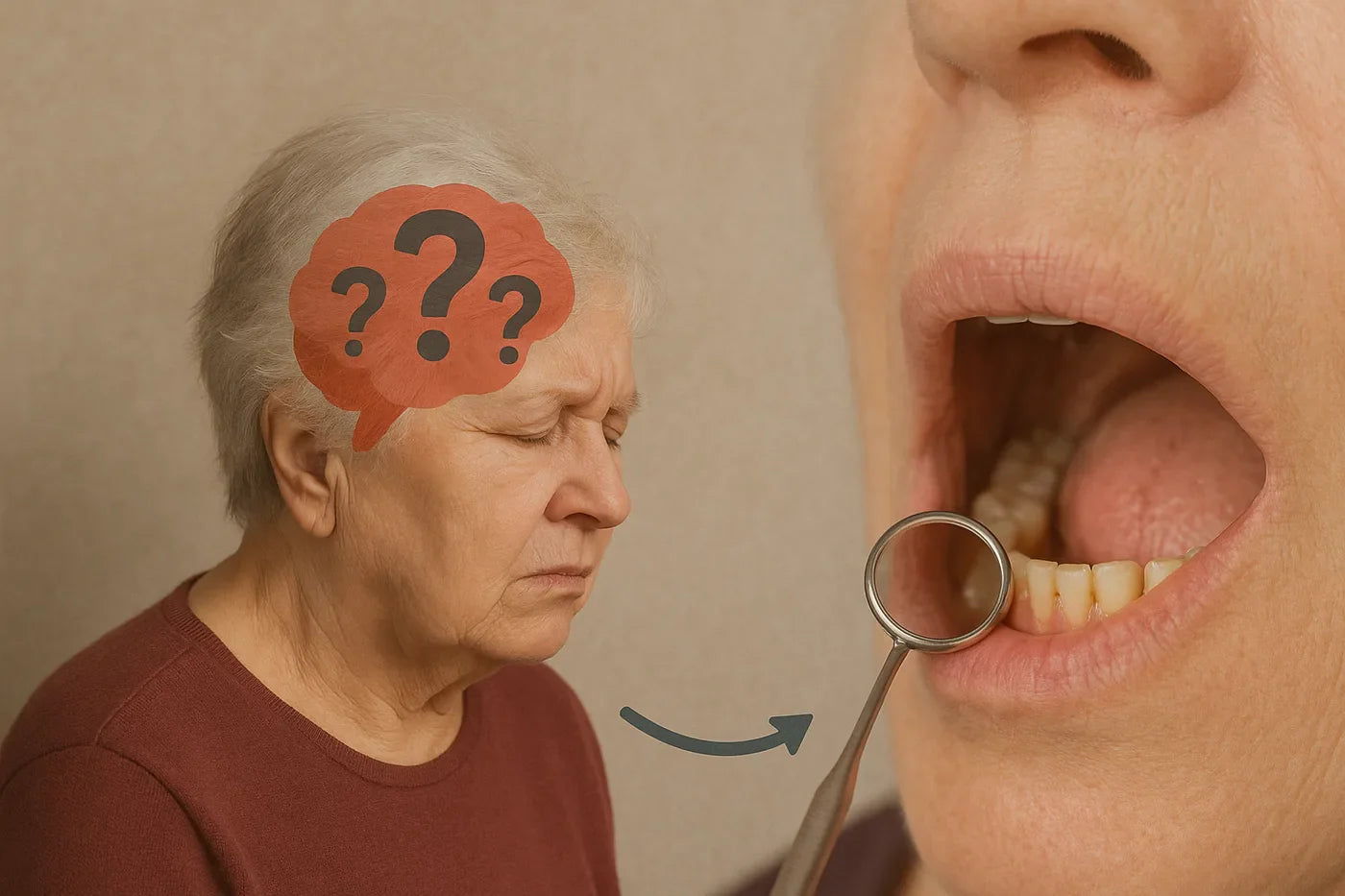
Supporting Oral Health with Cognitive Changes After Stroke
Essential Takeaways
- Cognitive changes after stroke consistently lead to poorer oral health outcomes. Structured reminders, visual cues, and caregiver support help maintain oral hygiene routines during recovery.
Understanding Cognitive Changes and Oral Health After Stroke
Cognitive changes are among the most common complications following stroke, affecting a significant portion of survivors both in the acute phase and during long-term recovery. These changes don't just impact daily activities. Research consistently demonstrates they significantly affect oral health maintenance, creating documented risks for dental and overall health complications.
The connection between cognitive impairment and poor oral health outcomes in stroke survivors is well-established in the scientific literature, though researchers note that more targeted intervention studies are needed to optimize specific support strategies.
Common Cognitive Challenges Affecting Oral Care
- Forgetting to brush teeth or floss daily
- Unable to remember the last time oral care was completed
- Difficulty recalling proper brushing techniques or duration
Attention and Concentration Issues:
- Getting distracted mid-brushing routine
- Rushing through oral care without proper technique
- Difficulty focusing on thorough cleaning of all mouth areas
- Problems planning and organizing oral care routines
- Difficulty initiating self-care activities independently
- Trouble sequencing steps in proper order (brush, floss, rinse)
- Impaired decision-making about when oral care is needed
The Research: Cognitive Changes and Oral Health Outcomes
Documented Health Risks
Multiple research studies consistently demonstrate that stroke survivors with cognitive impairments face significantly higher rates of gum disease, dental plaque accumulation, and tooth decay compared to those without cognitive challenges. Recent systematic reviews confirm strong associations between cognitive deficits and poor oral health outcomes in this population.
Key research findings include:
- Consistently higher rates of periodontal disease in cognitively impaired stroke survivors
- Increased dental plaque accumulation due to inadequate oral hygiene routines
- Greater difficulty maintaining regular dental care and professional cleanings
- Higher prevalence of untreated dental disease in stroke patients with cognitive changes
- Elevated risk of aspiration pneumonia from poor oral hygiene
The Cognitive-Oral Health Connection
Poor oral health in cognitively impaired stroke survivors creates a dangerous cycle: oral bacteria can contribute to systemic inflammation, potentially worsening cognitive decline and increasing the risk of recurrent stroke events.
(Microorganisms, 2024)
Evidence-Based Strategies for Supporting Oral Health
Research validates the need for structured, practical interventions to support oral care among stroke survivors with cognitive changes. While more randomized controlled trials are needed to evaluate specific intervention components, clinical studies consistently show that comprehensive support programs including education, structured routines, and caregiver involvement. Improve oral hygiene outcomes in this population.
Technology-Assisted Reminders
Digital Solutions:
- Smartphone alarms with specific oral care labels ("Time to brush teeth")
- Calendar reminders with step-by-step instructions
- Smart home devices programmed with daily oral care announcements
- Medication reminder apps that include oral hygiene tasks
Visual and Audio Cues:
- Talking alarm clocks with recorded personalized messages
- Visual timers to ensure adequate brushing duration (2 minutes)
- Color-coded schedules posted in bathroom areas
Environmental Modifications
Visual Cue Systems:
- Leave toothbrush and toothpaste in prominent, consistent locations
- Bright colored toothbrushes to increase visual salience
- Step-by-step picture guides posted near bathroom mirrors
- Checklist cards laminated and placed by the sink
Research supports the use of environmental modifications and visual cues as effective strategies for supporting self-care routines in individuals with cognitive impairments. Clinical guidelines frequently recommend these approaches for addressing cognitive deficits after stroke.
Bathroom Organization:
- Simplify choices by keeping only essential oral care items visible
- Consistent placement of all oral hygiene supplies
- Good lighting to support visual processing
- Non-slip mats and grab bars for safety during routines
Caregiver Support Strategies
Caregiver Support Strategies:
- Gentle verbal prompts without taking over the task completely
- Modeling behavior by brushing teeth together
- Positive reinforcement when routines are completed
- Consistent timing to establish habit patterns
Clinical research supports the involvement of caregivers in oral health maintenance for stroke survivors with cognitive deficits. Studies demonstrate that structured caregiver education and support programs lead to measurable improvements in oral hygiene practices and outcomes.
Graduated Support Approach:
- Full assistance during acute recovery phase
- Hand-over-hand guidance as cognitive function improves
- Verbal prompting with visual supervision
- Independent completion with periodic check-ins
Adaptive Equipment and Techniques
Modified Tools:
- Electric toothbrushes with timers and pressure sensors
- Larger-handled toothbrushes for easier gripping
- Foam toothbrushes for sensitive mouths or limited mobility
- Pre-threaded floss picks to simplify flossing
Simplified Routines:
- Break complex routines into single-step instructions
- Focus on essential activities first (brushing before flossing)
- Use all-in-one products when possible (whitening toothpaste vs. separate steps)
Timeline and Recovery Expectations
Cognitive recovery after stroke varies significantly among individuals. Oral care support needs typically evolve through several phases:
Acute Phase (0-3 months):
- Maximum support needed for all self-care activities
- Focus on preventing oral health deterioration
- Professional oral care may be required
Sub-acute Phase (3-6 months):
- Gradual return of some cognitive functions
- Introduction of reminder systems and environmental modifications
- Increased independence with continued supervision
Chronic Phase (6+ months):
- Establishment of long-term support systems
- Focus on maintaining independence with minimal assistance
- Adaptation to permanent cognitive changes if present
Advanced Technology for Cognitive Support
For stroke survivors with cognitive changes, modern smart oral health technology can provide valuable support by reducing the mental load required for effective oral care. Advanced devices like the Feno Smartbrush offer comprehensive cleaning that addresses many of the challenges associated with cognitive impairments after stroke.
Benefits for Cognitive Challenges:
- 20-second full-mouth cleaning reduces the need to remember complex brushing patterns and sequences
- Brushing action eliminates concerns about proper technique or adequate duration
- 18,000 bristles working simultaneously ensures thorough cleaning even when attention or focus is compromised
- Built-in oral scanning technology provides objective health assessments when self-monitoring abilities are limited
Reducing Cognitive Burden: Traditional oral care requires multiple executive function skills planning the sequence, timing the duration, coordinating movements, and assessing completeness. Smart oral health devices can automate many of these processes, allowing stroke survivors to maintain excellent oral hygiene with less cognitive demand.
While these technologies don't replace professional dental care or eliminate the need for caregiver support, they can serve as valuable tools for maintaining consistent oral health when cognitive changes make traditional routines challenging.
When to Seek Professional Help
Contact healthcare providers if you notice:
- Persistent neglect of oral hygiene despite reminder systems
- Significant decline in cognitive function affecting self-care
- Signs of oral infection or severe gum disease
- Difficulty swallowing or managing oral secretions
- Resistance or agitation during oral care attempts
- Safety concerns during bathroom routines
Key Takeaways for Stroke Survivors and Families
Remember: Cognitive changes affecting oral care aren't character flaws. They're common neurological consequences of stroke that can be successfully managed with proper support systems.
Start early: Implementing cognitive support strategies as soon as possible prevents oral health deterioration and establishes helpful patterns.
Be patient: Cognitive recovery takes time, and oral care abilities may fluctuate during the healing process.
Stay flexible: Adapt strategies as cognitive function changes, maintaining the balance between support and independence.
Seek help: Professional guidance can optimize both cognitive recovery and oral health outcomes.
Conclusion
Cognitive changes after stroke present real challenges for maintaining oral health, but they don't have to result in dental deterioration. Through evidence-based reminder systems, environmental modifications, appropriate caregiver support, and professional guidance, stroke survivors can maintain excellent oral hygiene throughout their recovery journey. The key is recognizing that cognitive support for oral care isn't temporary assistance. It's an investment in both immediate oral health and long-term overall wellness.

Feno Founders Edition Bundle
Advanced Oral Health in 20 Seconds with the Feno Smartbrush™
Get Yours Now!





